55 year old male with decompensated CLD
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
CONSENT WAS TAKEN FROM BOTH PATIENT AND ATTENDERS
55 year old male patient was brought to casualty with complaints of
scrotal swelling since 15 days
Fever since 15 days
Cough with sputum since 15 days
Yellowish discoloration of eyes since 15 days
Shortness of breath since 15 days
History of presenting illness
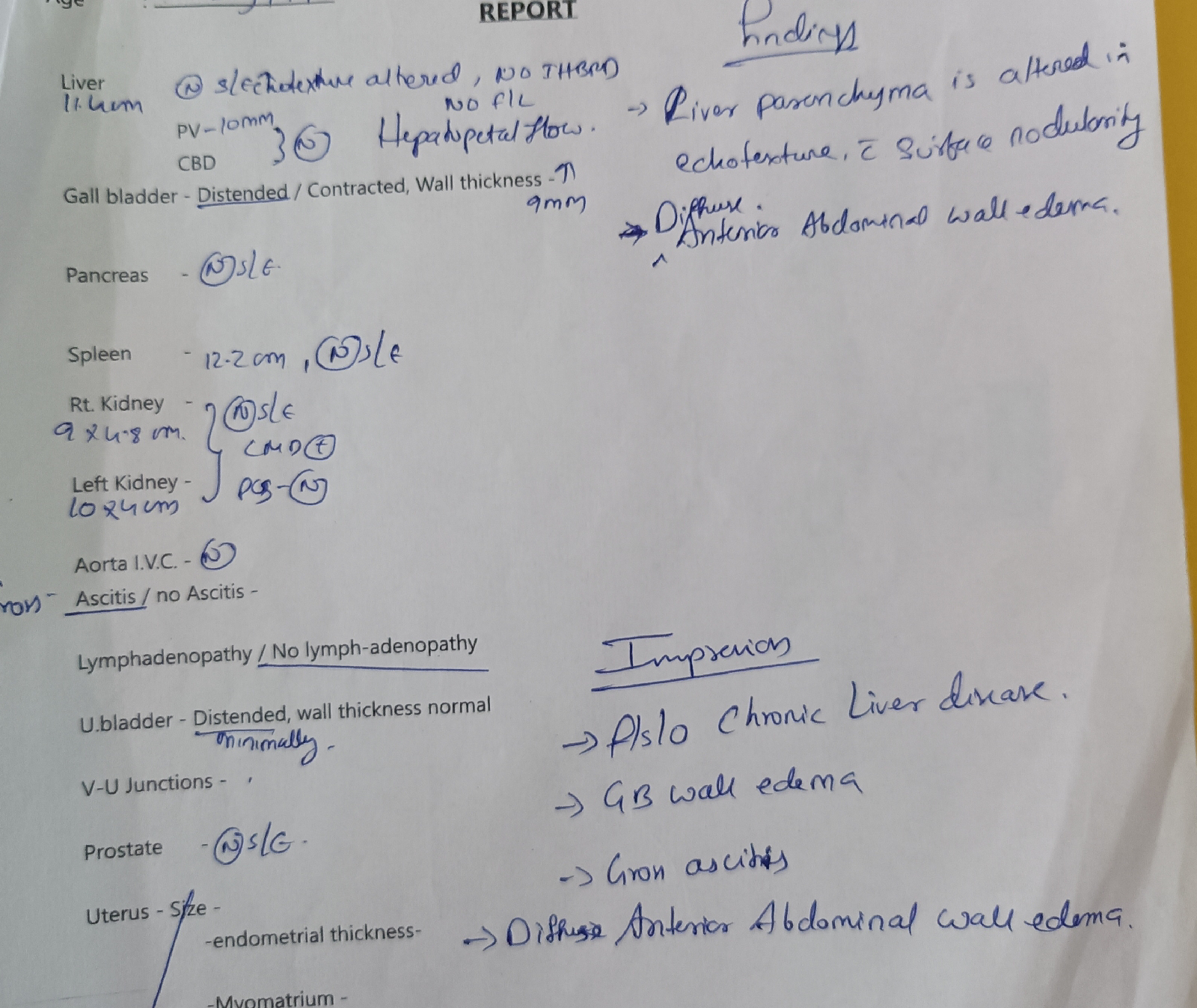
Patient was perfectly alright 6 months back when he developed abdominal distension which was insidious onset, gradually progressive , associated with shortness of breath and bilateral pedal edema,not associated with pain, no aggrevating and relieving factors.
H/o melena present
He was then diagnosed with chronic liver disease , endoscopy was done which showed grade 2 esophageal varices. Ascites was managed by therapeutic tapping.( around 8 litres of ascites fluid was tapped)
Since 15 days,he developed bilateral scrotal edema , gradually progressive associated with dragging type of pain , local rise of temperature and redness present.
History of fever associated with productive cough
-No H/o hematemesis , bleeding per rectum, constipation.
-No history of orthopnoea, paroxysmal nocturnal dyspnoea.
-No history of epigastric and retrosternal burning sensation
-No history of facial puffiness, decreased urine output , hematuria .
-No history of confusion, drowsiness or altered sleep rhythm.
-No history of diabetes, asthma, tuberculosis,CAD, CVA, epilepsy
On examination
Patient is conscious coherent and co operative
Pallor present
Icterus present
No cyanosis,clubbing, generalised lymphadenopathy.
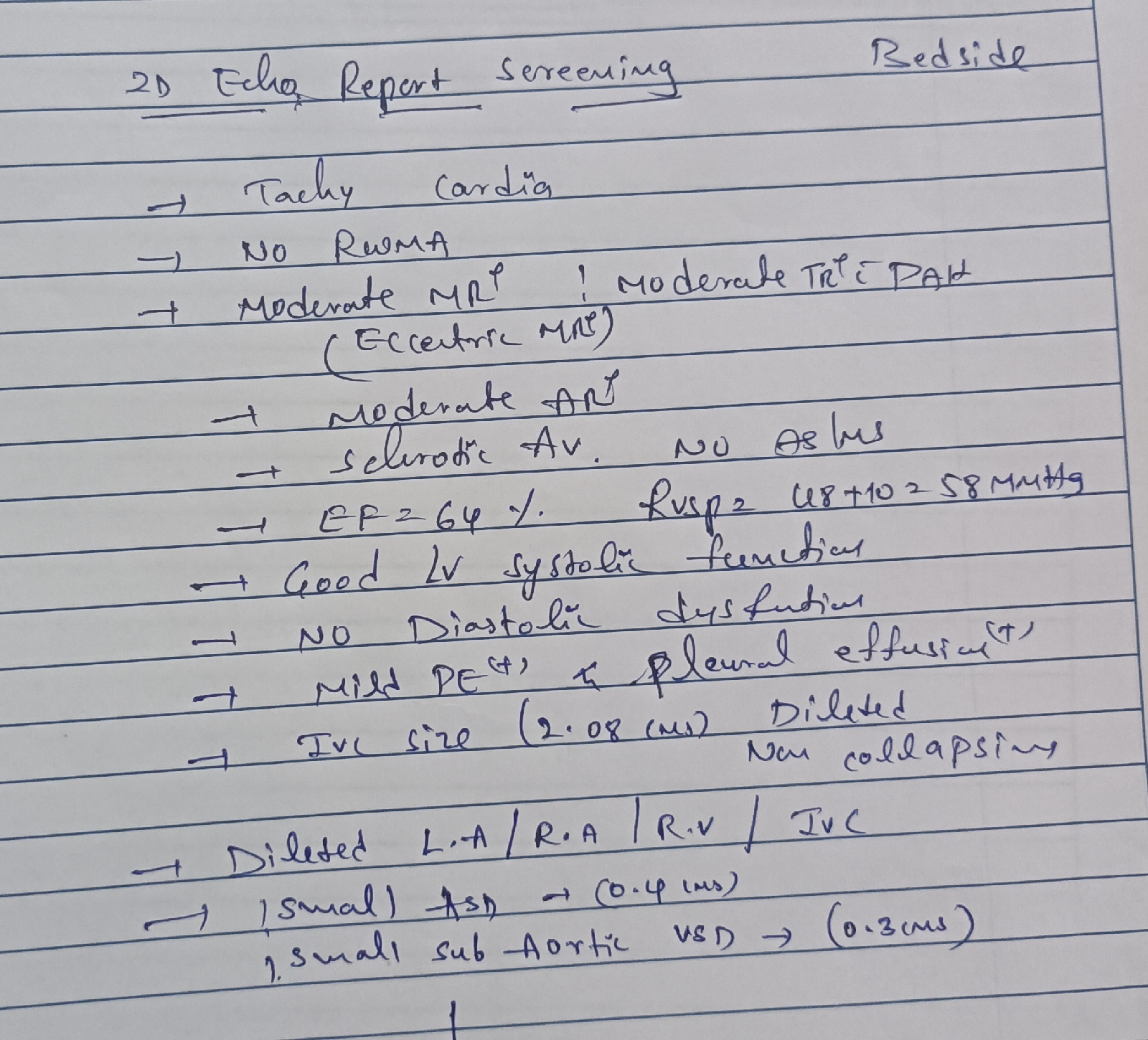
jvp showing prominent x and y descent
Vitals
Bp 110/70 mm Hg
PR 80 bpm
Rr 16 cpm














Comments
Post a Comment