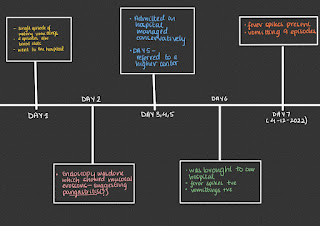
20year old with fever and vomitings
No history of burning micturition.
No history of productive cough , breathlessness.
No history of neck stiffness.
No history of pain abdomen, loose stools.
No history of weight loss.
PAST HISTORY
No similar complaints in the past.
No history of diabetes, hypertension,asthma, tuberculosis, epilepsy.
PERSONAL HISTORY :
he has been staying at home past one year after completion of his training in ITI .
His daily routine :
he wakes up at 8:00 am in the morning, gets fresh up and takes breakfast occassionally and goes out with friends
then comes home and skips his lunch most of the time and sleeps and then goes out with friends in the evening and comes home at 10:00pm and has his dinner by 11:00pm
He consumes tea or coffee 10 to 20 times a day
No history of alcohol consumption or smoking.
FAMILY HISTORY:
No significant history in the family.
GENERAL EXAMINATION:
patient is conscious, coherent and cooperative , well oriented with time, place and person
He is moderately built and nourished
He has no pallor
Icterus
Bulbar conjunctiva clear
No clubbing
No generalised lymphadenopathy
No pedal edema.
A single palpable lymph node is present in the right upper cervical region, which is soft in consistency, about 1.5 cm size and slightly mobile.
He has two tattoos( becomes significant if serology turns out positive)
Vitals :
Temperature:
PR :101 bpm
Bp : 110/90 mm Hg
RR: 18 cpm
SYSTEMIC EXAMINATION:
ABDOMINAL EXAMINATION
INSPECTION
- Shape - Scaphoid, with no distention.
- Umbilicus - central in position, normal
- Equal symmetrical movements in all the quadrants with respiration.
- No visible pulsation,peristalsis, dilated veins and localized swellings.
PALPATION
- Local rise of temperature present.
NO TENDERNESS
- Mild enlargement of liver,
regular smooth surface , rounded
edges , non tender.
- SPLEEN
palpable just below the costal margin,
smooth , rounded margins, non tender.
PERCUSSION
- Hepatomegaly : liver span of 14 cms with
3 cms extending below the costal margin
- Fluid thrill and shifting dullness absent
AUSCULTATION
- Bowel sounds not heard.
-No bruit or venous hum.
NO LOCAL LYMPHADENOPATHY.
CNS
Higher mental functions intact.
No signs of meningeal irritation.
Normal sensory examination
Normal motor examination.
Cerebellar signs are absent.
CVS :
S1 S2 heard, no murmurs.
RESPIRATORY SYSTEM
Bilateral air entry present, Normal vesicular breath sounds on both sides.
PROVISIONAL DIAGNOSIS
Fever under evaluation
Gastritis ( due to associated risk factors)
My differentials for fever
? Viral Hepatitis
? Typhoid
? Malaria
INVESTIGATIONS
CUE
LFT
SAMPLES ARE SENT FOR
WIDAL TEST
BLOOD CULTURE
URINE CULTURE
Repeat sample for serology
TREATMENT:
NIL BY MOUTH
MONITOR VITALS
INJ PAN
INTRAVENOUS FLUIDS :
RL
NS
INJ NEOMOL 1gm SOS (if temperature is above 101 degree)
Tab DOLO 650 MG PO TID
Data on association of tea and gastric acid release:
(to explain his pangastritis )
https://pubmed.ncbi.nlm.nih.gov/6546540/
Quoting the main lines :
Gastric acid response to a 200-ml cup of tea was measured by in situ titration in 36 patients with duodenal ulcer (DU) and 56 without duodenal ulcer (controls). Tea resulted in an acid secretory response which was almost equal to that after a maximal dose (0.04 mg/kg) of histamine. The effect of tea was mainly due to its local chemical action on gastric mucosa.
My questions regarding this case:
Do dietary habits alone show association with gastritis? Or should H pylori be ruled out?
How common is acute gastritis ( like in this case) associated with H pylori?
How can we be sure that gastritis and the fever, positive examination findings are separate entities?
Is there a need to rule out viral gastritis? Does a CMV or HSV viral infection explain all his features?
What is the sensitivity and specificity of Rapid diagnostic tests of HCV?
Are there any case studies of hepatitis C and acute gastritis?
I have found cases of chronic autoimmune gastritis, in hepatitis C patients, but doesn't fit in this case.



















Comments
Post a Comment